
Online test
Find out the severity of your symptoms with this free online test
Dermatillomania, or excoriation disorder is a complex disorder with no definitive cause for onset. If you investigate what triggered the of onset in a sample group of people who compulsively pick their skin, the conclusions will vary from modelling a family member to stress, neuro-imbalances to anxiety. One often overlooked possibility is the link with sensory processing. Sensory integration has been thought to be associated with body focused repetitive behaviors (BFRBs), whereby the act of picking the skin, pulling the hair or biting the nails provides a form of sensory input that either dampens an overstimulated brain or stimulates an understimulated one. The concept of sensory seeking behavior is not new. In 1972 occupational therapist Jean Ayres defined the term sensory integration as "the neurological process that organizes sensation from one's own body and from the environment and makes it possible to use the body effectively within the environment". When a person has difficulty with any aspect of that process, it is classified as a sensory processing disorder or SPD. Coincidentally the same initialism is used for dermatillomania, also known as skin picking disorder (SPD).
The role of sensory modulation disorder in dermatillomania
There are three subtypes of SPD, namely sensory modulation disorder, sensory-based motor disorders and sensory discrimination disorder. In sensory-based motor disorders disorganized processing results in problems with balance, motor planning, coordination, postural control and/or endurance. As the name suggests, sensory discrimination disorder is when the individual struggles to make sense of the sensory input they are receiving. It may take them longer than average to determine exactly what they’re looking at, hearing, or feeling. Sensory modulation disorder describes a group of individuals who struggle to process and regulate the sensory input they receive in terms of intensity, frequency duration, complexity, and novelty. This particular subtype of SPD is further divided into another 3 subtypes:
- Sensory over-responsivity
- Sensory under-responsivity
- Sensory craving/seeking
Over-responsivity is when the individual experiences a heightened sensory input, regardless of the level of sensory stimulation received, which results in stress to the body. This can then compel the individual, without even being aware, to seek sensory inputs to counter this effect on the body, known as sensory soothing behaviors. Conversely, sensory under-responsivity is the when the individual experiences a dampened sensory input, leading to sensory seeking behaviors. In seeking sensory stimulation, people tend to go to the sites where there are many nerve endings. Hands, feet, mouth and the scalp are common places. It would thus stand to reason that skin picking, nail biting, cheek biting, nose picking, and hair pulling - all body focused repetitive behaviors (BFRBs), be targets for sensory seeking behaviors. Touching, rubbing, pickng and pulling at the skin or perceived imperfections of the skin provides tactile stimulation.
Implications for treatment
Although there is a very likely link between SPD and dermatillomania, research and scientific evidence into this connection is lacking. It is also important to make the distinction that dermatillomania is not a sensory processing disorder, but rather that the presence of a sensory processing disorder may precipitate its onset. Research suggests that there are wide differences in the way individuals experienced the condition so there is no one treatment fits all recipe. Dr Penzel, a prolific expert and researcher in the fileld of BFRBs, recommends the use of Dr. Masuetos comprehensive treatment approach, which addresses the biological, behavioral, and cognitive needs of each patient to build recovery plans that they can maintain. However, establishing a link with sensory processing in an individual client opens up the possibility of a range of clinically proven treatments in sensory integration, often provided by sensory integration specialists.The first step is to identify whether the individual is seeking stimulation or sensory soothing and in response to what stimuli. This will enable the person to pre-empt these situations so that they may find ways to block or replace skin picking with less destructive sources of stimulation or self-soothing. It is recommended that further research be conducted in to the link between sensory processing disorder and BFRBs such as dermatillomania, and an investigation into the potential role of sensory integration occupational therapy in the treatment of these disorders, particularly among children and teens.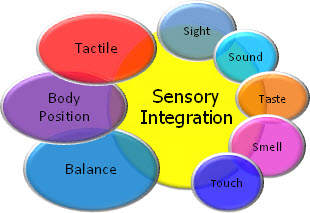
Online test
Find out the severity of your symptoms with this free online test
Start your journey with SkinPick
Take control of your life and find freedom from skin picking through professional therapy and evidence-based behavioral techniques.
Start Now



