Glossary
Compulsive Skin Picking (CSP) is a disorder associated with varying symptoms, categorized under several disorder types, and treated with many methods. This glossary provides additional information about CSP and defines related terms. We explain each term as it relates to CSP, to shed more light on its origin and treatment.
Anxiety

Anxiety is a feeling of unease, such as worry or fear. However, when feelings of nervousness or anxiousness become excessive or impair functioning, then it may be disordered. This blog post talks about the difference between everyday anxiety and disordered anxiety. While some anxiety is healthy, too much anxiety can interfere with quality of life.
Anxiety disorders comprise multiple disorders. Key diagnostic features for anxiety disorder is an abnormal response disproportionate to the situation, and the anxiety interferes with daily life. Often, anxiety disorders originate from fear, trauma, genes, environmental stress, or a prolonged stress response to a real, perceived, or unknown danger. Each person experiences anxiety differently, therefore a thorough assessment by a qualified professional is required before treatment.
Types of anxiety disorders include:
- Generalized anxiety
- Phobias
- Panic disorder
- Agoraphobia
- Social anxiety disorder
Although stress and trauma disorders have their own category in the new Diagnostic and Statistical Manual, conditions such as acute stress disorder and posttraumatic stress disorder involve symptoms of anxiety.
Approximately 30% of adults experience an anxiety disorder in their lives. Anxiety disorders often interfere with sleep, appetite, attention, concentration, memory, emotional functioning, and relationships. Skin picking is highly correlated with anxiety with many people reporting increased picking behaviors in response to anxiety. In other words, picking the skin can trigger anxiety, anxiety can trigger picking behaviors, or both. Most people who engage in treatment for skin picking also address issues related to stress and anxiety.
Body dysmorphic disorder (BDD)
Body dysmorphic disorder (BDD) is a condition where someone becomes preoccupied with a perceived or real defect of appearance. The fixation on the defect often leads to repetitive behaviors aimed to correct it. The thought of the abnormality causes severe distress and functional impairment.
Most people with BDD are normal or exceptionally good looking. Others perceive the flaws of attention as inconsequential, however the person with BDD cannot recognize or minimize the perceived seriousness of it.
Skin picking and BDD often get confused during diagnostic assessment because many people with BDD pick at their skin to remove perceived imperfections. The pivotal difference between the two is that in BDD, the cause of picking is the perception of defects and picking is a means to remove the defect or imperfection. In compulsive skin picking, the behavior is the focus of the disorder. The two disorders share additional symptoms including:
- Preoccupied with appearance
- Overly concerned how others judge their appearance
- Repetitive mirror checking
- Compulsive skin-touching, to measure or feel the perceived defect
- Social withdrawal
- High levels of self-consciousness,
- Repetitive grooming behaviors
- Constant mental comparisons about appearance
Approximately 1.9% of the population experience BDD, yet 73% of those with BDD target the skin. Although treatment interventions include medications and cognitive-behavioral therapy, the completed suicide rates in people with BDD is 45 times higher than in the general population of the United States.
Cognitive Therapy
Cognitive Therapy is psychotherapy, or talk therapy, based on the assumption that the way people think affects emotions. The interaction between therapist and client focuses on the identification of distorted or unrealistic ways of thinking in the present. There are multiple forms of cognitive therapy, but the goal is to address current problems, not analyze the past, and determine how current thinking patterns affect emotion and communication. Cognitive therapy is one component of the more widely used cognitive behavioral therapy The interaction between therapist and client is one of guidance where the therapist helps the client identify thought patterns through probing questions. Then, the treatment goal is to interrupt or change maladaptive thought patterns that contribute to skin picking behaviors. Cognitive therapy for skin picking may focus on the thoughts that lead to the behavior such as thoughts the lead a person to remove skin perceived as imperfect. Length of treatment time varies based on client needs, but cognitive therapy was designed to be a short-term therapy, usually taking three to six months.
Dermatologist
A dermatologist is a medical doctor specializing in the diagnosis and treatment of skin diseases involving the skin, hair, nails, and mucous membranes. The name comes from the word "derma" which is the scientific term for skin. A dermatologist may treat skin picking disorder's physical effects including treating wounds, healing scars, alleviating skin irritation, and prescribing medication. A dermatologist may also rule out physical causes for skin picking disorder including allergies, hypersensitivity or other physical causes. Doctors familiar with psychodermatology also understand the connection between stress and the skin. Although dermatologists do not treat the psychological aspects of the disorder, they are an integral member of the treatment team.
Head banging
Head banging is a stereotypic movement or rhythmic movement disorder commonly found in infants or young children. Considered a soothing repetitive motion, researchers believe the movements relieve tension and promote relaxation, especially since children often do it before they fall asleep. This form of head banging typically involves repeated banging the head against a pillow, mattress, or headboard. Head banging might also help children express frustration. The behaviors typically dissipate by age 5.
Though head banging disorder is usually attributed to children, it also occurs in adults usually as a sleep behavior known as rhythmic movement disorder.
Head banging describes a form of dance, performed while listening to music, particularly rock and heavy metal music. Though it is hard to see an underlying connection between head banging in children and the head banging "dance", one might find a relationship between the two in that both activities involve repetitive movement, from which people feel pleasure. This type of pleasure is sometimes called the kinesthetic drive or the joy in movement that all humans share.
Impulse control disorder
Impulse control disorders such as skin picking disorder, kleptomania, pyromania, pathological gambling, trichotillomania, and intermittent explosive disorder are conditions where a person cannot control an impulse or urge which results in impairment or behaviors that harm themselves or someone else. Core components of an impulse control disorder include repeated engagement in the behavior despite its harmful or negative effects, lack of control over the behavior, a consistent urge to engage in the behavior, and positive feelings while engaging in the behavior. Compulsive skin picking may fall into this category of disorders.
Neurotic (Psychogenic) excoriation
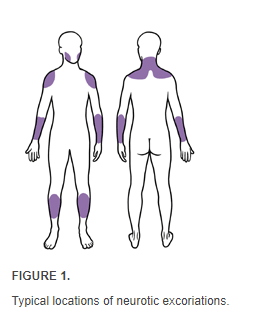
Neurotic (Psychogenic) excoriation is a medical term used by physicians to refer to repetitive scratching with no known physical pathology. The behavior manifests on the skin as “clean, linear erosions, scabs, and scars…similar in size and shape…grouped on easily accessible body sites.” The most common areas affected by neurotic excoriation include the legs, arms, shoulders, upper back, neck, and face.
Image from American Family Physician
The terms “neurotic” or “psychogenic’ mean that the condition is psychologically motivated rather than physical. However, a differential diagnosis of neurotic excoriations will include ruling out physical causes. Physicians note that some physical conditions such as dry skin, allergies, delirium, hepatic disease, substance use, medication side effects, and thyroid issues may cause neurotic excoriation, but more often the behavior occurs with depression, anxiety, or obsessive-compulsive disorder. There are other cases where neurotic excoriations start with a physical condition but continue long after treatment of the physical causes.
Dermatological treatments may include topical antibiotics to prevent infection of the scratch wounds, topical steroids to facilitate healing and antihistamines to reduce sensations related to itching. When physicians encounter a patient displaying symptoms of neurotic excoriations, the best practice is to refer the patient to counseling to address the psychological origins of the behavior.
Psychiatrist
A psychiatrist is a medical doctor trained and certified to treat mental illness. Psychiatrists are mental health professionals who may prescribe psychiatric medication as part of the treatment process. Psychiatrists conduct physical examinations, diagnosis psychiatric conditions, and provide treatment which may include psychotherapy, medication, or other treatments such as ECT. Although the biological cause of skin picking disorder remains unknown, research indicates some people benefit from pharmacotherapy.
At one time, psychiatrists were the only providers who could prescribe medication. However, because of psychiatrist shortages in some areas of the United States, some states allow psychologists to obtain prescriptive authority through special training and licensing. Also, some psychiatric nurses may prescribe in some states. Always verify the licensing and credentials of providers prescribing medication.
Psychodermatology
Psychodermatology is the study and practice of the relationship between skin disorders and psychology with dermatologists understanding the role of the “skin-brain connection.” Many skin disorders have an underlying emotional cause. As the largest organ in the body, the skin contains a dense network of nerve cells sensitive to stress and tied directly to the sympathetic nervous system which activates during the stress response. Further, the skin connects to the endocrine system which is also involved in the expression of stress and anxiety. Therefore, psychodermatologists consider the role of stress and other psychological disorders as causes for skin conditions and the effects of skin conditions. Increased awareness of this connection makes psychodermatologists integral to someone in recovery from skin picking disorder. Read more in the blog post about psychodermatology for skin picking disorder.
Psychotherapist
A psychotherapist is a practitioner who uses interpersonal communication to help clients with emotional, mental, or behavioral problems of living and usually includes increasing an individual's sense of well-being and reducing discomforting experiences. Psychotherapists use a variety of techniques through dialog and communication to improve the mental health of a client or to improve group relationships (such as in a couple or family). Psychotherapy can address the emotional and behavioral aspects of skin picking disorder, ease stress and anxiety that result from the disorder, and help clients talk about problems.
The term “psychotherapist” does not indicate the practice license held by a provider. States or other governmental authorities grant licenses that give a provider the authority to treat clients for particular conditions, regulated under a scope of practice. Psychotherapist is a general term and may include psychiatrists, psychologists, professional counselors, clinical social workers, or psychiatric nurses. Therefore, before engaging the services of a psychotherapist, verify that the provider holds a verified license to practice.
Most providers who use the term psychotherapist do so to describe what they do. However, most differ from psychiatrists in that they cannot treat or diagnose physical or medical aspects of illness nor can they prescribe medications. Only a medical doctor can perform these functions although some states allow psychologists to prescribe medication, but only with a special license.
Serotonin
Serotonin is a neurotransmitter which plays an important role In the central nervous system by carrying messages bidirectionally in the brain and the digestive system. It helps regulate autonomic functions, anger, aggression, body temperature, mood, sleep, vomiting, sexuality, and appetite. It is often called the "happiness" chemical because it contributes to making us feel good and comfortable. Skin picking is sometimes associated with serotonin imbalance and medications that restore serotonin levels can help treat the disorder.
Skinorexia
Skinorexia is a synonym for Compulsive Skin Picking (Dermatillomania). This term first appeared online in 2010 according to Google Trends. Accordingly, a skinorexic is a person who has skinorexia. Skinorexia is not an accepted medical term because it implies similarity to anorexia which is not supported by the evidence.
Substitution therapy
Substitution therapy is a term used to describe a harm reduction treatment for opioid use disorders where safer versions of the drug substitute for the unsafe, illegal forms. The most common types of substitution therapy are methadone and buprenorphine. However, the term can also refer to a treatment modality for skin picking disorder, where the client learns to replace skin picking behaviors with a different activity, such as physical exercise or creative activities as painting or writing. This technique may benefit people whose underlying psychological energy accumulates and picking relieves the tension. Redirecting this energy towards positive activities can not only free the person from harmful behaviors, but create positive results for quality of life.
Trichotillomania
The origin of the term Trichotillomania (TTM) is from Greek: Trich - hair, Till - pull, Mania - madness

Hair pulling (Trichotillomania) is a disorder characterized by pulling hair from the body at the root resulting in significant hair loss. The most affected part of the body is the scalp (head), however other places where hair grows are affected as well (eyebrows, beard, pubic hair, nose hair, eyelashes etc). This disorder is classified under same category as compulsive skin picking. Indeed, the two disorders are closely connected and often researched together since they both involve the connection between a compulsive urge and a body-focused repetitive behavior.
Approximately 2% of the population has trichotillomania which often begins around puberty, with females experiencing the disorder up to four time more than males. While the cause remains unknown, medical research suggests that heredity, genetics, hormones, and stress can contribute to developing the disorder.
Like skin picking disorder, trichotillomania is a body-focused repetitive behaviors (BFRB) often confused with non-suicidal self injury, body dysmorphic disorder, and most commonly, obsessive-compulsive disorder. However, BFRBs differ in that they are behavior-driven, start early in adolescence, and involve repetitive motor symptoms relating them closely with tic disorders. Most notably, the medications that show effectiveness with cognitively driven disorders such as OCD do not work with BFRBs.
People with trichotillomania endure the physical effects of hair loss, damaged hair follicles, skin damage, and possible infections. For those who eat the hair after pulling it, further digestive complications arise. Psychologically, people with trichotillomania feel high levels of shame, humiliation, embarrassment, anxiety, and low self-esteem often leading to social isolation and other impairments.
Trichotillomania treatment is similar to skin picking disorder and includes physical, psychological, and social interventions. Read more about this disorder on our trichotillomania website.