Dermatillomania: All you need to know about skin picking disorder
What is Dermatillomania
Also known as excoriation disorder, or skin picking disorder (SPD), dermatillomania is a body-focused repetitive behavior (BFRB) where someone recurrently and compulsively picks at their skin to the point of injury. Dermatillomania behaviors include repetitive touching, rubbing, scratching, picking at, and digging into the skin and can target healthy or unhealthy skin, scabs, lesions, pimples, or other blemishes. Most people who suffer from this disorder pick at the face, arms, and hands. Some people use tools to poke, squeeze or lance the skin. Resulting injuries include skin discoloration, scarring, infections and in the most severe cases, severe tissue damage.
The origin of the term Dermatillomania is from Greek: "derma" - skin; "till" - pull; "mania" – madness.
Dermatillomania is a multisyllabic word that slides off the tongue with rhythm. In some ways, it is a fun word to say out loud because it’s long yet easy to pronounce. However, the word itself reveals an appropriate picture of the disorder.
Dermatillomania is a disorder that affects the skin, thus the inclusion of "derma" in the word. Derma is another word for dermis which indicates the skin and comes from Greek. None of the skin on the body is off limits to a patient with this disorder. The second portion of the word contains "till," which means to pull in Greek. Think of pulling a plow behind a horse, cow, or tractor to break open the soil for planting.
Research has not yet defined a specific cause that leads an individual to pick uncontrollably and destructively. Some theories point to trauma, illness, chemical or hormonal imbalance, violence, abuse, neglect, perfectionism, emotional dysregulation, and very low self worth. Perhaps the person suffering from dermatillomania is subconsciously plowing away at the older, outer layer of spent skin in order to find a fresher, livelier person beneath. In today's vernacular, "mania" is often associated with crazed psychotic behavior that adds chilling drama to big-screen movies. Indeed, there was a time, in ancient Greece, when mania simply meant madness.
Dermatillomania, then, translates to mean someone who has an illness that produces an overwhelming desire to pick, pull, and plow away at his or her own skin, even though they know it's painful, unsightly, and almost impossible to justify.
Types of Behaviors
The skin picking behaviors of dermatillomania present differently based on the individual differences in each person.
Automatic
- Picking occurs without consciously doing so
- Occurs when someone is bored or not focusing
Focused
- Picking responds to a drive
- Triggered by stress, anxiety, boredom, or tension
- Physical sensation precedes picking, such as tingling, discomfort, or an itch
- May begin with a goal of correcting a skin imperfection
- After picking, a person may feel relieved or pleasure, but the urge to pick returns
Furthermore, the behavior patterns and sometimes the underlying motives for the behaviors, vary depending on the area of focused picking.
- Compulsive face picking rarely starts with a visible problem. Someone experiencing this may pick at an area without any noticeable imperfections, but over time, persistent picking may lead to visible wounds. This may cause feelings of discomfort or embarrassment, leading the person to avoid social situations, which in turn may contribute to increased stress and anxiety. For some, compulsive face picking may become a way to cope with difficult emotions or feelings of unworthiness.
- Scalp Picking involves finding blemishes and imperfections at the scalp. They can be imagined or real, but with persistent scratching and pulling a person will develop wounds on the head, which becomes a valid target for more scratching and picking, creating a vicious cycle hard to break. When taken to the extreme, this behavior can even cause bald spots.
- Picking at the acne often starts during the teenage years, when hormonal changes can cause an outbreak of pimples. Teenagers tend to have issues with self-esteem as they transition from childhood to adulthood, and the onset of acne can make those issues worse. Although they think picking the acne will get rid it, the opposite often occurs. The most important problem with skin picking acne is that it can cause infection, skin discoloration, and scarring.
- Lip picking consists of peeling, biting, or chewing the skin on or around the lips. While many people often pull or bite off a bit of peeled skin on their lips, compulsive lip pickers go beyond that. Driven by stress, boredom, or worry, they cause so much harm to their lips that bleeding and injury occurs and ordinary activities, such as eating or kissing, feel unpleasant or even painful.
- Nail picking involves biting, chewing, and picking one's nails and cuticles. Again, it is normal to bite or pick off damaged bits of nails that get stuck on whatever a person is handling, but when it becomes a matter of biting and picking until the nails, cuticles, or surrounding skin bleed, it's a sign of dermatillomania. Students suffering from nail picking often stop during school breaks, only to start over when they return to a stressful environment.
- Picking scabs can start as a coincidence. A person can have a scab caused by an accident and start picking at it. If it comes when the person is under stress or vulnerable, the picking may have a soothing effect. Then it becomes a self-perpetuating behavior that relieves anxiety and makes the person feel more anxious because the constant picking is painful.
Regardless of where the skin picking occurs on the body when it becomes excessive and causes injury, it is often a sign of disorder and may require professional assistance.
Online Test for Skin Picking
How Severe is Your Picking Disorder? Find Out With This Free Online Test
Take the testOnset, Prevalence, and Course
Dermatillomania can start at any time throughout the lifespan, but it most often starts between the ages of 9 and 13 at the start of puberty. One recent study of those with Dermatillomania showed that over 47.5% of those interviewed started to exhibit skin picking behaviors before the age of 10.
It begins for many reasons. For many patients, skin picking first began by scratching and picking at acne, but the compulsion to scratch and pick the skin continues even after the acne has vanished. Other types of skin conditions such as keratosis pilaris, psoriasis, and eczema can also act as a trigger. Grooming the skin with these conditions can be normal. However, those with dermatillomania exhibit excessive grooming disproportionate with the severity of the skin condition.
Another common age of onset is 30 - 45 years old. Onset at this age can occur for similar reasons such as acne and other skin conditions. It is also related to stressful life events and including marital conflicts, the death of friends or family, and unwanted pregnancies. Skin picking behaviors may also begin after a traumatic brain injury. Dementia is a degenerative brain disease which changes the brain physically. As parts of the brain degrade, the parts that control repetitive movements change structurally resulting in repetitive body movements. Examples include hand flapping, moving appendages, and even skin picking.
There is also evidence that dermatillomania can begin with medication. A recent article described a case where someone developed skin picking disorder after receiving treatment with methylphenidate for ADHD. Methylphenidate is a stimulant to the central nervous system used to treat hyperactive and impulsive ADHD. It acts by blocking the reuptake of neurotransmitters in the prefrontal cortex that contribute to impulsivity. Research suggests it may be useful for treating the impulsivity that accompanies skin picking disorder, but this case suggests that using stimulants can also backfire.
According to the Diagnostic and Statistical Manual of Mental Health Disorders 5th edition, 1.4% of the population suffers from dermatillomania. However, more recent findings suggest it affects between 2% and 3% of the population and three-quarters of them are female. Due to the shame and embarrassment associated with the disorder, many choose not to report it. Therefore, the prevalence of dermatillomania could be significantly higher.
The course of dermatillomania throughout the lifespan is chronic and cyclical. When it begins in early adolescence, it can be a confusing and disturbing experience. Especially when someone tries to stop and they do not understand why they cannot. At this age, the pressures of internal and external stigma cause stress on overall mental health which can make the urge to pick even worse. In many cases, as the person grows older and learns what it is, they seek treatment, accept the disorder, and learn how to recognize triggers and to choose other behaviors. While the disorder lasts a lifetime, people learn to manage the behaviors and to recognize triggers that correlate to more picking.
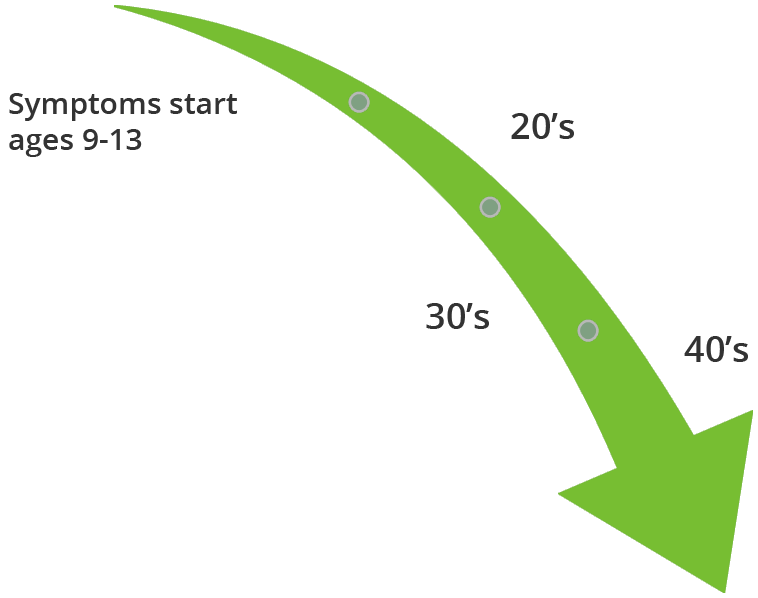
Symptoms Severity Decreases Over the Lifespan
Correlates and Causes
The exact cause of dermatillomania is unknown, but neurologic theories provide insight. A cause is something directly connected with the disorder such as a physical abnormality or environmental trigger.
Correlates are associations. Meaning certain conditions occur more in people with dermatillomania which gives an indication of relatedness but relatedness does not mean cause. For example, lack of physical activity is correlated with poor cardiac health. Yet, there are plenty of people with low physicial activity who have good cardiac health and others with poor cardiac health who get plenty of exercise.
Correlates
Heredity
Research suggests that dermatillomania, like other BFRBs, is more common in people who have family members with similar disorders such as OCD (obsessive-compulsive disorder) or another BFRB (body-focused repetitive behavior). Although just having a family member with one of these disorders does not mean someone will develop dermatillomania. Research suggests there is a hereditary correlation, but not a cause.
Obsessive-compulsive disorder
There is a relationship between obsessive-compulsive disorder (OCD) and skin picking disorder. Skin picking is considered a disorder on the OCD spectrum of disorders and they are often mistaken for each other. About 8-21 percent of individuals who have OCD will have a co-occurring skin picking disorder. However, in one study, people with skin picking disorder were more likely to have co-occurring body-repetitive behaviors such as nail biting or trichotillomania while people with OCD were more likely to have co-occurring body dysmorphic disorder.
Anxiety and Depression
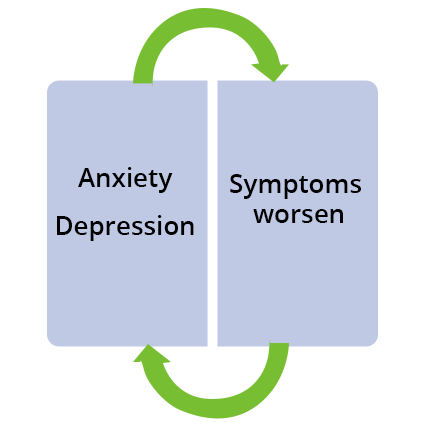
Anxiety and depression are strongly correlated with skin picking disorder. Multiple studies found that people with high rates of anxiety experienced more severe skin picking symptoms. The same occurs with depression. These findings are consistent in the research; however, it seems to be a cycle of behavior and anxiety intermingled with skin picking behaviors where it is difficult to discern which causes the other. Picking may trigger anxiety, anxiety trigger picking, or both. Many experts agree that the initial trigger does not matter, only that treatment should include addressing anxiety and depression as well as skin picking.
Shame
Shame is a negative evaluation of self that affects mood, thoughts, and behaviors. Shame is not just a negative evaluation of behavior or habit. The negativity surrounding a behavior or habit is generalized to the whole person, and one ends up feeling like a bad person because they engage in a behavior. Those who experience shame tend to socially isolate, hide feelings and behaviors, and have higher severity of symptoms not only of skin picking disorder but anxiety and depression. Shame also increases suicide risk and functional impairment.
Impulsivity
In research, there are multiple types of impulsivity. Attentional impulsivity is the ability to keep attention on something while motor impulsivity is the ability to control behavior. Some people with skin picking disorder do so because they have trouble with impulsivity. Those with skin picking disorder who score high on attentional and impulsivity measures are more likely to have more severe picking behaviors. While neuroscience continues to work on finding ways to counter impulsivity through medicine, there are cognitive behavioral therapies that focus on the distinct types of impulsivity.
Hormones
The first-time symptoms of skin picking start during a significant hormonal change in the body. Also, a study of 1,471 women aged 10-60 found a relationship between hormonal changes and an increase in “focused” picking behavior. These women described picking behavior as more severe when hormones were changing throughout their lives. To the body, hormonal changes are stressful, and many other mental health issues are affected by them. Research from the World Health Organization suggests hormonal changes involved in perimenopause, or the 2-8 years before menopause, can cause mood and anxiety symptoms to worsen. Therefore, if hormone changes can worsen mood and anxiety symptoms, it can be assumed that skin picking behavior tied to anxiety may also worsen.
Thyroid
Thyroid hormones manage homeostasis of the skin. If the thyroid malfunctions, the skin is unable to regulate itself.
There are four major thyroid malfunctions:
- Hyperthyroidism - the thyroid produces too much hormone
- Hypothyroidism - not enough hormone, or the body is unable to use the hormone
- Structural abnormalities - the gland is too large or too small
- Tumors on the thyroid
The skin is a complex organ that consists of thyroid receptors throughout its multiple layers. The mechanisms by which all this occurs is complicated and affected by genetics. However, to simplify, thyroid hormones tell skin when to grow, how to grow, and how hair should grow. Skin also takes direction on moisture and redness from the thyroid hormones. When thyroid hormones are out of balance, the skin reacts. When the skin receives too much thyroid hormone, the skin increases in smoothness, moisture, and warmth. The skin may itch, grow red, and manifest hives. When thyroid levels are too low, the skin may turn yellow, decrease in temperature, and dry out which leads to calcification or dry, scaly skin. When this happens, dry, scaly skin can crack open, and the wounds take much longer to heal.
Thyroid and Stress
Thyroid hormones and stress also have strong links. The thyroid gland works in tandem with the adrenal glands which regulates cortisol in response to stress. When a person handles stress well, the adrenal glands release a bit of cortisol to enhance the body until stress resolves. Cortisol slows down thyroid function. Think of when anxiety hits and what happens to your skin. Do you ever get nervous and your hands feel cold, clammy and dry? That is a short-term version of thyroid hormone reduction. However, if stress recurs often, the body’s metabolism slows, and thyroid hormone levels drop.
Stress
Stress and skin picking are closely related. Multiple research studies found that those with skin picking disorder and high rates of stress experienced more severe symptoms and people with severe picking behaviors report increased stress. Skin picking also causes increased stress due to the damage caused by the skin and the stigma associated with the disorder. Many people with this illness pick at their skin causing damage to multiple layers of skin. Without treatment, skin wounds can lead to scabs, scarring, and infections leaving visible evidence often observed but misunderstood by others. The body reacts to the physical damage by releasing more cortisol and thyroid hormone to heal the wounds but also risks overload causing the slower metabolism, low thyroid hormone production, and slow wound healing. Then the person is stuck with wounds that are difficult to hide.
Skin Conditions
There are many triggers for compulsive skin picking, but some of them are physical. For example, some people who pick at their skin start by trying to correct an imperfection. Sometimes the flaws are blemishes, and sometimes they are invisible to all except the person plagued with the compulsion. In other cases, sensations such as itching or burning of the skin inspire picking behavior, and when the picking behavior reduces the physical sensations, the cycle will continue each time the sensation occurs. Other times, the compulsion to pick is aimed at scabs or the breaks in the skin caused by dryness and cracking.
Causes of Dermatillomania
The cause for dermatillomania is unclear. One of the most common hypotheses is that skin picking is an impaired stress response. When a person is experiencing elevated levels of turmoil, arousal, or stress, they cope with it by picking at their skin. Research reinforces this hypothesis because the action appears to be maintained by automatic self-reinforcement in the person exhibiting the behavior. Though most scientists agree that the causes of dermatillomania are firmly rooted neurologically, there are those that believe it is associated with one’s environment. Many psychologists believe that those with skin picking disorder do it because of repressed rage or other unexpressed feelings. Additionally, studies have shown a correlation between dopamine and the desire to pick the skin.
Dermatillomania signs and symptoms
There are clear criteria set out by the Diagnostic and Statistical Manual 5 (DSM5) for the diagnosis of skin picking disorder. These guidelines include:
Recurrent skin picking resulting in skin lesions
People with skin picking disorder have a compulsion to pick their skin frequently, often resulting in tissue damage, sometimes even infection. The impulse or urge to pick is so strong, some describe the experience as similar to that of a substance addiction.
Repeated attempts to decrease or stop skin picking
One of the main differentiating criteria between dermatillomania and other conditions like obsessive compulsive disorder (OCD) and body dysmorphic disorder (BDD) is that the person is cognitively aware that the picking is undesirable and therefore tries to stop picking. One of the signs of a skin picking disorder is therefore a history of failed attempts to stop picking.
The skin picking causes clinically significant distress or impairment in social, occupational, or other important areas of functioning
Despite the instant gratification experienced when picking, the person is acutely aware that what they are doing is destructive, and this causes them great distress. A key symptom of skin picking disorder is that immediately following picking, the person experiences intense shame and guilt about their behaviour. There is a desire to stop picking, but the inability to resist the impulse to pick, and this further reiterates feelings of guilt, as well as feelings of failure. Another sign is that often the impulse to pick encroaches on the person’s day to day functioning, particularly in severe cases when picking occurs more frequently. Skin pickers often report spending large amounts of time picking, causing them to be consistently late or to miss social events all together. In cases where the person experiences the urge to pick strongly at a time when they are unable to pick (e.g. in the company of others) they may find it difficult to concentrate. The damage caused by the skin picking is also a great source of embarrassment and shame, often resulting in the individual avoiding social situations where their scars may be more visible such as the beach, poolside or gym. In severe cases the person may become completely isolated from society in an attempt to prevent others seeing the damage they have caused to their skin. Another sign of this is that people with skin picking disorder often dress inappropriately for the weather. When the picking site is on the arms, neck or legs, attempts to hide these areas are made by wearing turtle necks or long sleeves despite the hot weather.
The skin picking is not attributable to the physiological effects of a substance (e.g., cocaine) or another medical condition (e.g., scabies)
Some substances induce a physiological reaction on the skin such as itching or burning. If the person repetitively scratches at an itchy skin, this is not recognised as a skin picking disorder. If however, after the physiological skin condition subsides and the person continues to pick or scratch at the site, a skin picking disorder may have developed.
The skin picking is not better explained by symptoms of another mental disorder
Some mental disorders result in psychosis characterised by tactile hallucinations. In these cases the person experiences a physiological reaction on the skin which is not there, such as the sensation of something crawling on the skin, itching or burning. This can lead to repetitive scratching, rubbing or picking to the point of tissue damage. In these instances, skin picking disorder is considered a diagnosis. Other conditions such as body dysmorphic disorder cause the person to have perceived flaws in their physical appearance which causes them psychological distress. In these cases the person may repetitively pick at the skin in an attempt to remove the perceived imperfection. This behaviour is therefore not viewed as destructive in purpose. Skin picking disorder also bears a striking resemblance to non-suicidal self-injury. However in these cases the person consciously intends to harm the body. People with skin picking disorder may consciously pick at the skin, but never with the view to harm the body, although this inevitably does occur. The desire to stop picking is therefore a fundamental criterion for the diagnosis of dermatillomania. Finally, stereotypic movement disorder whereby the person displays a pattern of repetitive stereotypical behaviours may also often present with skin picking, rubbing or scratching. The presence of this diagnosis is also an exclusionary factor when querying a diagnosis of dermatillomania.
Classification of the Disorder
Dermatillomania is categorized within a group of disorders called Body-Focused Repetitive Behaviors (BFRBs). However, it is often confused with other conditions. Common misdiagnoses result because the picking behavior is a result of a medical condition, confused with OCD, Body Dysmorphic Disorder (BDD) and in some cases, Non-suicidal Self-Injury (NSSI).
Medical Conditions
A few of the medical conditions that also cause skin picking include eczema, psoriasis, diabetes, liver disease, Hodgkin’s disease, polycythemia vera, systemic lupus, and Prader-Willi syndrome.
Drugs
Drugs including cocaine and methamphetamine are known to cause uncontrollable picking and itching in users. Drug users may pick at the skin for several reasons, including the sensation of something crawling on or under the skin, also known as formication. When the effects of the drugs wear off, so do picking behaviors.
Obsessive Compulsive Disorder (OCD)
There are cases when a person with OCD picks at their skin and cases where people with dermatillomania have OCD. However, the main difference is that the behavior of picking drives someone with dermatillomania not intrusive or obsessive thoughts. Whatever stimulates the urge, once picking occurs, the urge is satisfied. On the other hand, a person with OCD may feel a compulsion to pick their skin but the drive behind it will be intrusive or obsessive thoughts. After the person picks, the thoughts will still be there.
Another theory is that dermatillomania is a repetitive motor response. Behaviors associate with OCD are compulsive rituals essential to satisfying an obsession. The age of onset is also different. Dermatillomania usually starts in early adolescence while OCD usually starts in late adolescence. OCD and BFRBs are treated differently even though they share some clinical characteristics outlined above. Selective serotonin reuptake inhibitors (SSRIs) help in treating OCD but in people with dermatillomania, they do not work as well.
Dermatillomania
- Behavior-driven
- Repetitive motor symptom
- Starts in early adolescence
- Habit Reversal treatment
- SSRIs not effective
OCD
- Thought-driven(obsessions)
- Compulsive ritual
- Starts in late adolescence
- Exposure and response prevention treatment
- SSRIs effective
Body Dysmorphic Disorder (BDD)
A person with body dysmorphic disorder is obsessed with a defect in their physical appearance which can be real or imagined. Sometimes people with BDD will pick at their skin excessively, but the picking is directed at the perceived defect. For someone with dermatillomania, the goal is not to fix a defect. It may start out that way, but the compulsion to pick is the main driver of behavior.
Non-suicidal Self-Injury (NSSI)
When a person hurts themselves without suicidal intent, it is called non-suicidal self-injury (NSSI) and can include cutting, burning, or scratching. Theories about NSSI believe it is thought to serve a purpose for relieving devastating negative emotion, punishing oneself, demonstrating anger toward oneself, or for influencing others. While there are similarities between focused dermatillomania and NSSI, NSSI is a purposeful decision to hurt oneself as opposed to the compulsive urge to pick.
Effects
Physical Effects
- Lesions and wounds in areas of frequent picking
- Most common include the face, arms, legs, back, lips, stomach, chest, shoulders, and scalp
- Fingernails, cuticles, and toenails are often picked
- Infection at the picking site.
- Tissue damage with some cases severe enough to warrant skin grafting
- Permanent scarring
- Physical disfigurement
Psychological Effects
- Helplessness
- Guilt
- Shame
- Embarassment
- Anxiety
- Depression
- Suicide
Treatment
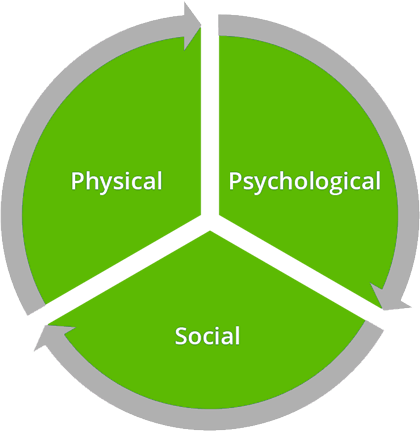
Sadly, very few people with dermatillomania, between 30% and 45%, seek treatment. Although it is a lifelong, chronic condition which means that medical science has no cure, treatment is possible. It takes time and consists of learning how to manage triggers, urges and behaviors affiliated with skin picking. Treatment needs to include the physical, psychological, and social aspects involved with the behaviors. Recovery is a whole-person, whole-lifestyle endeavor which works on behavior management, emotional regulation, and thought management. It also works with people on the effects of shame, embarrassment, and stigma. A social network of encouragement from others who struggle with similar disorders allows for an exchange of information and innovative coping strategies.
Dermatillomania that goes undiagnosed or confused with other mental disorders often results in more harm. Seek an expert in body-focused repetitive behaviors (BFRBs) when looking for a therapist. They know how to properly assess for behaviors and triggers, and they have knowledge about the latest evidence-based treatments. They also understand that everyone experiences the disorder differently and can guide you through improving your self-awareness to identifying the types of treatments that will work for your unique situation.
Physical
- Learn self-awareness to identify urges, triggers, and behaviors.
- Care for your body internally by eating a healthy diet.
- Care for your body externally by allowing damaged skin to heal properly.
- Develop strategies to manage urges, triggers, and behaviors.
- Create way to manage stress.
Talk to your doctor about medications and supplements that could help.
Selective Serotonin Reuptake Inhibitors (SSRIs) show effectiveness for managing OCD and some people with dermatillomania report satisfactory results. Doxepin, clomipramine, naltrexone, olanzapine, and pimozide all may be useful in the reduction of skin picking behaviors, but clinical studies have not shown unmistakable evidence due to the lack of randomized controlled trials.
Take Care of Skin. Keep skin healthy
- Avoid harsh chemicals on the skin.
- Avoid temperature extremes.
- Avoid stressing the skin.
- Moisturize.
- Prevent infection.

Post-picking skin care
- Cleanse
- Keep skin, hands, and tools clean before and after picking.
- Avoid harsh chemicals to treat wounds.
- Use gentle cleansers that will not cause inflammation
- Soothe
- Some dermatologists recommend using a toner with antiseptic properties to remove any remaining germs or bacteria.
- Treat open wounds with Neosporin to prevent infection.
- Hydrate
- Moisturize with a light, chemical-free moisturizer to protect the skin while it’s healing.
Psychological
- Find a therapist. Several therapeutic interventions show positive results including cognitive behavioral therapy, habit reversal training, acceptance and commitment therapy, and comprehensive behavioral therapy. Although they are not evidence-based practices, some people report positive outcomes from hypnosis, group therapy, and alternative treatments.
- Address mental health issues like self-esteem, anxiety, stress, depression, trauma, or relationship difficulties.
- Consistently practice self-care.
Social
- Connect with people who support and care for you.
- Ask them to be part of your recovery.
- Look for and join a support group in person or online.
- Learn from others how they cope with urges and manage behaviors.
- Use what you learn to help others.
For detailed treatment options, see our Dermatillomania Treatment page.
Dermatology
Dermatologists are physicians who specialize in treating conditions of the skin. Dermatillomania tends to result in visits to a dermatologist to get help with problems from chronic skin damage. How often do dermatologists recognize a compulsive body-focused repetitive behavior and refer a patient to a therapist or psychiatrist for help?
What dermatologists know
During training, dermatologists are taught about the interconnectedness between the skin and the nervous system. Not only do some skins condition worsen during periods of heightened nervous system activity such as stress and anxiety, but skin conditions often provide fuel to heighten the nervous system. In dermatology, the interconnection between the skin and the psychosocial dimension of skin conditions is called psychocutaneous medicine. Despite receiving initial training, many dermatologists neglect the role of psychology.
The good news is that there are clinics that offer psychodermatology and treatment for psychocutaneous disorders, but they are rare. Dermatologists can help their patients by recognizing the connection between mental health issues such as anxiety, depression, OCD, and psychosis, all recognized as factors in other skin disorders such as vitiligo, psoriasis, and dermatillomania. Showing patients that they understand by validating a patient’s experience is powerful for those who reach out for treatment for skin lesions that result from picking. Creating an open environment where people do not have to hide their picking behaviors will facilitate earlier treatment and less skin damage. Second, they can educate patients to take care of their skin and finally, dermatologists can refer their patients to mental health professionals who specialize in body-focused repetitive behaviors.
