Dermatillomania Treatment Options
Dermatillomania is a mental health disorder that is often misdiagnosed and not understood. Those who struggle with it tend to go untreated which makes the psychological and physical effects more severe.
Psychological Effects
- Isolation
- Embarrassment
- Feeling like a fraud
- Self-loathing
- Feeling alone
- Feeling crazy
- Shame
- Low self-esteem
- Depression
- Anxiety
- Hypersensitive to the reactions of others
- Hopelessness
- Fear of judgment
- Increased risk of suicide
Physical Effects
- Skin Lesions
- Scabs
- Discolored skin
- Scarring
- Tissue Damage
- Infections
- Physical disfigurement
Dermatillomania is a chronic condition, but treatment can help people learn to understand the compulsions behind it and manage the impulsivity and behaviors. Then, the disorder does not hold as much power over a person, reducing the feelings of helplessness. Those who struggle with dermatillomania all have different experiences. Treatment needs to apply to those individual differences, and qualified experts can help determine the best options.
Those with compulsive skin picking disorder also tend to struggle with other mental health disorders with some people becoming suicidal. Therefore, comprehensive treatment, or treatment for the whole person, will help address everything at one time.
Online Test for Skin Picking
How Severe is Your Picking Disorder? Find Out With This Free Online Test
Take the testCategories of Treatment
Cognitive Behavioral Therapy
The most common mode of treating body-focused repetitive behaviors is CBT (Cognitive Behavioral Therapy). It is a talking therapy that has been proved to help treat a wide range of emotional and physical health conditions in adults, young people and children. The main difference between CBT and other talk therapies is that the focus is more on how our thoughts and actions influence each other, and looking for strategies to alter that relationship so that the outcomes for both are positive; as opposed to reflecting on issues of the past. This method has the most research supporting it and the best outcomes. One of the reasons CBT is so effective is that it is applicable in a wide variety of settings, from individual face-to-face sessions, telephonic sessions, group therapy, self-help books and programs, and even text-based and online therapy programs. The practical and patient-driven nature of CBT allows it to be tailored to the specific needs of the patient or setting. However, CBT is a broad category of treatment and within that category are many specific interventions. The commonality between them is the assumption that thoughts, feelings, and behaviors are related to one another and therefore influence one another. For example, the thought of getting pulled over for speeding may trigger a feeling of fear. Therefore the person’s behavior complies with posted speed limits. While this is a simplified example, in reality, the process is complicated, and most people are not aware of the relationships between thoughts, feelings, and behaviors. A therapist trained to provide CBT can help people sort out the mess. For example, a person feels the compulsion to pick at their skin (behavior), however, after picking, they think “this is not good” which triggers feelings of shame and embarrassment, but the feelings trigger the compulsive behavior again. A person in this situation may feel helpless and unable to control the behavior.

However, CBT also counts on the idea that if a thought, feeling, or behavior changes, it will change the entire system. Therefore, in therapy, a qualified professional will guide someone through a process of becoming aware of the thoughts, feelings, and behaviors involved with picking and tackles a part of the system. For example, skin picking is a mental health disorder but does not define someone as a person. Acceptance of the disorder as a small part of oneself can help someone remove the judgment which causes the shame and embarrassment. Getting those feelings under control may prevent worsening of the cycle of picking behaviors. When the compulsions slow down, a person feels more in control of the behavior and then can make choices.
Read our comprehensive guide on how CBT works for dermatillomania if you want to know more about it. Or, if you already know enough to get started with your healing process, have a look at our online therapy programs:
Online Therapy Program
Get guidance and life-changing tools through our online platform and direct support from an expert therapist.
Find freedom from skin picking through a customized online program delivered by a therapist specialized in treating excoriation disorder.
Learn moreOur expert therapists will give you guidance and tools to help your child develop coping skills that address the day-to-day challenges of skin picking.
Learn more
Habit Reversal Training (HRT)
One type of CBT intervention targets behavior. Developed in the 1970’s, Habit Reversal Training has three parts:
- Increasing awareness. During this phase of treatment, a therapist helps someone observe their thoughts, feelings, and behaviors to determine patterns of when it happens, where it happens, how it happens, and what triggers it. This process of observation without judgment informs which treatment techniques will be appropriate.
- Find competing responses. In this phase, a person learns to do something that interferes with picking when the urge occurs. The interference is called a “competing response” and may include techniques such as wearing gloves, so a person cannot use their hands, or holding hands in a fist until the urge passes.
- The third aspect of HRT is social support. Most people with dermatillomania feel isolated and alone. Inviting supportive people into treatment can help a person by destigmatizing the disorder, countering beliefs about what others think, but supportive others can also help by giving positive feedback, recognizing patterns or triggers, intervening in an encouraging way, and sharing their observations. Social support also works the other way. May people with dermatillomania who share their experiences with others who have the disorder report positive feelings from being able to share what they learn with others.

HRT is an evidence-based practice. Research shows positive outcomes in short-term treatment but does not provide evidence of long-term success. Mixed results are partially because there is not a lot of studies specific to dermatillomania and long-term treatment outcomes. Read our complete guide on habit reversal training for skin picking to learn more about the treatment process.
Comprehensive Behavioral Treatment
When all of the available CBT treatment options are combined in a way that meets an individual’s needs, it is referred to as Comprehensive Behavioral Treatment. Therapists who use comprehensive behavioral treatment have access to many types of interventions which are then customized based on an individual’s particular disorder. There are four parts to this kind of therapy.
- Assessment. During this phase, the therapist and the individual build self-awareness through observation and self-monitoring much like the first part of HRT. They work together to identify thoughts, feelings, and behaviors that occur before, during and after picking which the individual deems problematic. When those aspects are identified, it provides an understanding of that person’s functioning.
- Substitute. The second phase includes creating sensory substitute behaviors that satisfy the urge to pick but prevent picking of the skin.
- Environmental alteration. This phase of treatment involves making the environment less friendly and less comfortable for picking.
- Emotional processing. The fourth phase of treatment involves the identification and processing of the negative thoughts, feelings, and emotions that people feel about their skin picking behaviors.
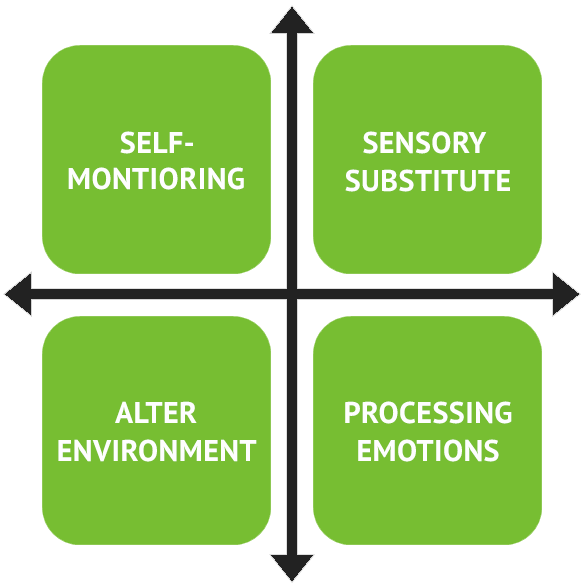
Comprehensive behavioral treatment occurs fluidly in that a person does not go from one stage to the next. While assessment needs to occur at the beginning to derive an understanding, the assessment also occurs throughout treatment as a way to evaluate what sensory substitutes work and which don’t, as well as if environmental alterations are effective or ineffective.
Acceptance and Commitment Therapy (ACT)
Another form of therapy for dermatillomania is Acceptance and Commitment Therapy (ACT). Pronounced ‘act,’ it is different from CBT because the goal is to learn how to accept thoughts and feelings as they are, even the negative ones. Where CBT teaches people how to control or change them, ACT does not. The process involves noticing, observing, experiencing, and accepting without judging oneself. One of the primary practices in ACT is mindfulness which helps people increase self-awareness as well as acceptance of negative and uncomfortable feelings. After acceptance, one can choose behaviors that coincide with what is important to them.

ACT treatment for people with dermatillomania involves allowing oneself to experience the urge to pick, accepting its presence, and then choosing not to do anything about it. As someone experiences the negative emotions that accompany picking, he or she can choose how he or she wants to respond, even if it means just accepting the negativity.
Hypnosis
In hypnosis therapy, a qualified trained professional enters the unconscious mind of someone with dermatillomania to draw out ways to help them managed the urges to pick. There is very little research to support hypnotherapy, but some people report positive outcomes. Additionally, this method could help people discover initial triggers of the disorder or help them deal with traumatic events that contribute to picking behaviors. Read our complete guide on hypnosis for skin picking disorder to see if it’s the right treatment for you.
Group Therapy
Many people with dermatillomania experience the disorder in isolation which can make behaviors worse. Group therapy is led by a therapist-facilitator and can be a viable option for those who want to engage in social support in a formal setting. One can participate in group therapy as the sole method of treatment or as an addition to individual therapy. Support groups are a less formal version of group therapy and are usually led by people who are not trained therapists.
Benefits of group therapy and supports groups:
- Learning from others.
- Universality – one is not alone
- No stigma – one can be themselves
- Sense of belonging to a group
- Shame or embarrassment decrease
- Support others by sharing experiences
Medication
There are no medications that specifically treat dermatillomania. However, there are some that research suggests handling some of the impulsivity, anxiety, depression, or stress that contributes to skin picking behaviors. By treating some of the things that make picking behaviors worse, people can experience a positive difference in treatment. Caution should be exercised with medications because some of them produce side effects that make picking behaviors worsen and each person reacts to medications uniquely. Therefore, even though a drug may work for one person with dermatillomania, it does not mean it will work for another.
One example is a class of medications known as selective serotonin reuptake inhibitors (SSRIs). Some people with OCD who take them report positive results, as do some people with dermatillomania. Examples that work include doxepin, clomipramine, naltrexone, olanzapine, and pimozide, but the evidence from research is not conclusive because there have not been randomized clinical trials for treating dermatillomania.
Another class of medication that can help are anti-itch creams or eczema and acne medications. These options can help people who pick at their skin because of itching or other physical sensations that prompt the behaviors. We covered in more detail potential medications for dermatillomania here.
Again, when considering medications, do so under the supervision of a trusted, qualified health professional who understands and treats patients who have body-focused repetitive behaviors.
Alternative Methods
Research provides options for treatment. However, there are other methods available. Dermatillomania is not fully understood by the medical or psychiatric field, therefore, many of these alternative treatment methods come from anecdotal evidence, or they are supported in some way by research that may or may not support their use.
USE CAUTION AND IN CONSULTATION WITH YOUR HEALTHCARE PROVIDERS.
Alternative therapies can interfere with medication or create unintended side effects or make picking behaviors worse.
Aerobic Exercise
- Anxiety or stress can make picking behaviors worse and exercise helps reduce anxiety or stress.
- Research showed adults who exercised for 6-12 weeks experienced fewer skin picking behaviors than those who did not exercise.
Acupuncture
- Research shows some positive outcomes for people with obsessive-compulsive behaviors.
- When used with therapy and medication, it showed decreased symptoms.
Aloe vera
- A topical application derived from plants or commercially available lotions.
- Can soothe uncomfortable physical sensations that can act as a trigger for picking.
- Can also be used in some cases to help heal the skin after picking.
Aromatherapy
- Some essential oils promote calm or soothe the skin.
- Use with caution since oils can be harmful to the eyes, nose, and broken skin.
Biofeedback
- This technique teaches people how to regulate body processes such as heart rate and body temperature.
- Learning to control processes usually thought to be automatic can help people learn how to attend to the triggers for picking.
- Biofeedback is noted as helping reduce stress and anxiety.
Chamomile tea
- Known as a calming tea which can soothe stress or anxiety.
Kava Kava
- Comes in supplement form or the leaves can be chewed.
- The plant has properties to aid in calming the body which can reduce picking behaviors.
Marjoram leaves
- Leaves can be chewed to calm the nerves during experiences of grief or shock.
- People who pick at their skin as a means of coping with stress report some positive effects.
Meditation
- Helps with stress reduction.
- Improves self-awareness and focus on the present.
- Builds skills to handle times of high anxiety or stress.
Yoga
- People with obsessive compulsive behaviors report more success when using yoga as a supplement to therapy than those who only used medication.
- Yoga stresses mindful breathing, controlled movements, and increased body awareness which can help people learn to focus on the present.
- Researchers looked at the brains of people who practice yoga and found differences in the regulation of emotion.
Reminder - Alternative therapies can cause unexpected side effects depending on a person’s neurochemistry and physiology. Discuss options with your healthcare providers first and report changes immediately.
Coping with Dermatillomania
Every manifestation of dermatillomania is different which means treatment needs to meet one’s individual needs. Comprehensive treatment considers the physical, emotional, and psychological aspects of compulsive skin picking. No matter which treatment intervention helps, there are ways to deal with having the disorder throughout the treatment process, and even work on reducing the urge to pick through changing some daily habits.
Awareness
- Observe and recognize emotional and behavioral conditions that accompany picking. For people who pick without conscious awareness, this step is essential.
- There is no one way to increase awareness. Many options exist - do not give up until you find one that works for you.
- Learning self-awareness takes time, so be patient. Ask for help when you need it.
- Be alert to signs that picking behaviors are related to other mental health issues such as anxiety or depression
Acceptance
- Dermatillomania is a mental health disorder, not a personal defect.
- Picking is a behavior that can be changed.
- Dermatillomania is not your fault.
Education
- Increase knowledge about dermatillomania, its causes, and correlates.
- Look for multiple treatment options.
- Learn from other people who learned to manage picking behaviors.
- Share with others. Educate those who do not understand the disorder to reduce stigma.
Use person-first language
- Instead of referring to yourself as a “picker” consider separating the behavior from your identity by saying “I struggle with dermatillomania.”
- Empower yourself. Research suggests practicing person-first language helps people feel more in control of the behaviors.
Enlist the support of others
- Isolation tends to increase the severity of picking behaviors.
- Invite close friends or family members into treatment with you.
- Use healthcare providers who have expert knowledge.
- Participate in support groups.
Lapse Management
Dermatillomania is chronic, which means it lasts throughout one’s lifetime. Treatment helps people manage the picking behaviors, but the urges do not go away. People who report success in treatment say that it helps them choose not to pick so the behaviors no longer interfere with their lives. Recovery is a journey that involves awareness, resilience, and perseverance, but sometimes the behaviors return. When that happens, some people refer to it as “relapse,” but that word can be reframed.
First, “relapse” has connotations associated with it that incite judgment, failure, fear and the definition in the dictionary does not help.
Relapse - suffer a deterioration after a period of improvement
However, consider the word “lapse…”
Lapse - to pass gradually into an inferior state or condition
Which has a more positive connotation to it. Just because someone reverts to picking does not mean he or she failed or deteriorated, it means they gradually went back to what they used to do. Language is important because it contains literal and nonliteral meanings. For example, someone with a medical condition like diabetes is not accused of having a “relapse” when their blood sugar spikes and people with dermatillomania do not deserve accusation either. Recovery is a challenge, and sometimes things happen. What matters is what you do when setbacks occur.
Get back up and take a step forward.
Lapse Prevention
- Expect lapses and plan for them.
- If you expect lapses to occur, they will not be accompanied by shock and negativity.
- Think in advance about high-risk situations, environments, or triggers which might set you back.
- Discuss these with your supportive others and your therapist. Brainstorm ideas of what you can do when it happens.
- Do not judge yourself.
- Keep yourself healthy
- Keep competing responses and grounding materials with you at all times so you can be prepared if urges strike.
- Live a balanced lifestyle, eat healthy, and exercise.
- Keep stress levels to a minimum and practice self-care.
- Keep routines, create competing responses, and maintain stimulus controls.
- Stay in touch with supportive others who can help you notice warning signs and encourage you.
Dealing with a lapse
- Take care of you. Do not beat yourself up with negative self-talk. Accept that it happened and move on.
- Get back up and move on.
- Return to the parts of treatment that worked including basic skills.
- Return to therapy if you need to or go back to a support group.
- Keep practicing skills for self-management.
- Evaluate.
- Assess what happened with your therapist or support person. Talk about what happened objectively.
- Create new plans for the future. Learn all you can from what happened by identifying the triggers and revising your coping skills.
As people age, life and environments change. What worked at the beginning of treatment may not work later. However, with recurring assessment, awareness, education, support, and perseverance, new ideas can support the treatment strategies you need for success.
